Incontinence: Laughing Off Life's Leaks
Incontinence is a pretty common issue, but it's surprising how little people talk about it. It's basically when you have accidental leaks of urine, and it's often wrapped up in unnecessary shame. Let's tear down those walls and offer support to those coping with it. Think of incontinence as more of a signal than a full-blown medical condition—it can be triggered by all sorts of things like your body, your emotions, or even your lifestyle choices. And while it tends to affect older adults and women more, it's definitely not limited to just them.
Alright, so when we talk about incontinence, there are actually a few different types you might come across. First up, there's stress incontinence, which happens when there's pressure on the bladder during activities like coughing, sneezing, or lifting heavy objects.
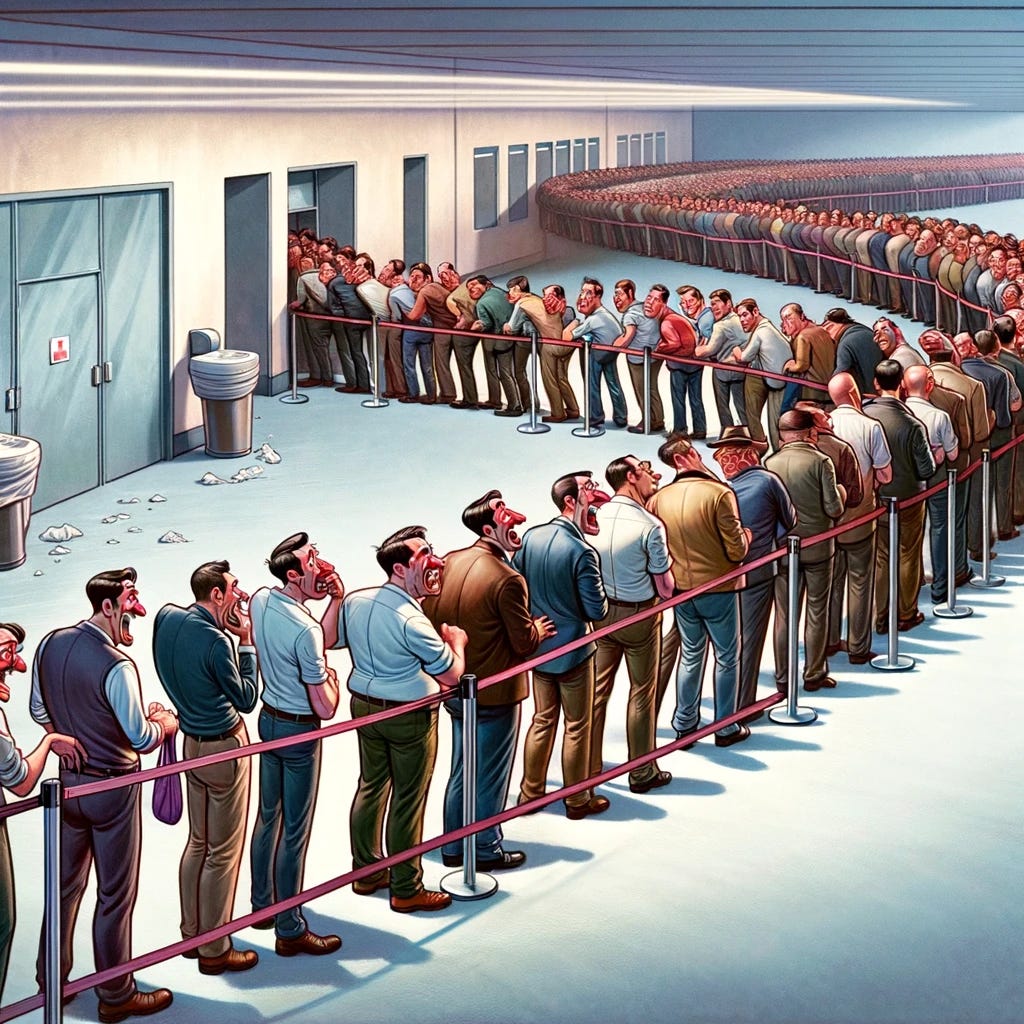
Then, there's urge incontinence, where you get this sudden, strong urge to pee and just can't hold it in.
Next, we've got overflow incontinence, which occurs when the bladder doesn't empty fully and ends up leaking.
Functional incontinence is another one—it's when physical or mental challenges make it tough to get to the bathroom in time.
And finally, there's mixed incontinence, which is a combination of stress and urge incontinence. These different types show how complex incontinence can be, which is why getting the right diagnosis and tailored treatment is super important.
When it comes to what causes incontinence, it's really a mixed bag. For women, stuff like pregnancy, giving birth, and hitting menopause can be big triggers. Men, on the other hand, might find prostate problems playing a role. And then there are other factors like getting older, being overweight, having diabetes, or dealing with nerve issues. Oh, and don't overlook lifestyle choices—what you eat and drink can impact how you handle it.
Breaking the silence surrounding incontinence is crucial because the stigma can lead to embarrassment, reducing quality of life and delaying seeking treatment. Understanding the type and cause of incontinence through a detailed medical history, physical exam, and possibly diagnostic tests is essential for effective treatment, which may include lifestyle modifications, pelvic floor exercises, medication, or surgical interventions in severe cases.
Lifestyle modifications for managing incontinence may include reducing caffeine and alcohol intake, maintaining a healthy weight, and practicing regular pelvic floor exercises. Additionally, establishing a consistent bathroom schedule and avoiding foods that irritate the bladder can also help alleviate symptoms.
Pelvic floor exercises, also known as Kegel exercises, involve contracting and relaxing the muscles of the pelvic floor. These exercises help strengthen the muscles that support the bladder, uterus, and bowels, thereby improving bladder control and reducing symptoms of incontinence. They are typically done by repeatedly contracting and relaxing the pelvic floor muscles in a controlled manner.
Alright, let's dive into the world of meds for handling incontinence. First up, we've got anticholinergics like oxybutynin and tolterodine—they're great at calming those bladder muscles, dialing back those sudden urges to go. Then there's mirabegron, another contender in the mix, which works on relaxing those bladder muscles, giving your bladder more room to hold on, and cutting down those frequent bathroom runs. And for the guys grappling with overflow incontinence due to prostate issues, alpha-blockers like tamsulosin could be the ticket. It's really about finding what works best for you and your specific situation.
There are minimally invasive procedures like injecting bulking agents around the urethra to help tighten things up and stop those leaks. And if things are a bit more serious, we might consider surgical options like sling procedures or placing an artificial urinary sphincter to give the urethra some extra support and beef up bladder control. The key here is that we tailor these interventions to fit your specific type and severity of incontinence, as well as your individual health needs and preferences.
With all the helpful tech available now, dealing with incontinence has become much simpler. Wearable devices and apps act like handy assistants, making pelvic floor training effortless, tracking bladder habits, and providing timely reminders when necessary. It's really about giving people more control and convenience in managing their bladder concerns.
Custom treatment plans that fit each person's needs can really make a difference—sometimes they can even completely sort things out. But it's not just about meds and procedures; it's also about rallying for more research and support, hooking folks up with support groups and counseling. As docs, we're not just here to treat—we're here to lend a caring hand, break down that stigma, and get folks talking openly about their urinary health.
Incontinence is something a lot of folks shy away from talking about, but it's actually pretty common. If we start opening up those conversations, we can really shift how we think about urinary health and make sure everyone dealing with it knows they're not alone. Having incontinence doesn't mean your life's on hold forever. With the right care and treatment, people can get back to living fully without always worrying about leaks. As urologists, our job isn't just about giving meds and treatments; it's also about being there with empathy and support, guiding folks through this journey with dignity and hope.